Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124

Know your mental health

Know your mental health

The connection between brain structure and behavior has long intrigued neuroscientists, but new research has shed light on an area of the brain that may play a surprising role in substance use. According to a recent study by Kohler et al, 2024, individuals with a thicker insula—a key brain region involved in emotion and decision-making—are more likely to increase their cocaine use when given a chance. This finding provides valuable insight into the neurobiological factors underlying addiction and opens up new avenues for prevention and treatment strategies.
In this blog, we’ll break down the science behind the study, what the findings mean for addiction treatment, and how this research might influence future mental health care.
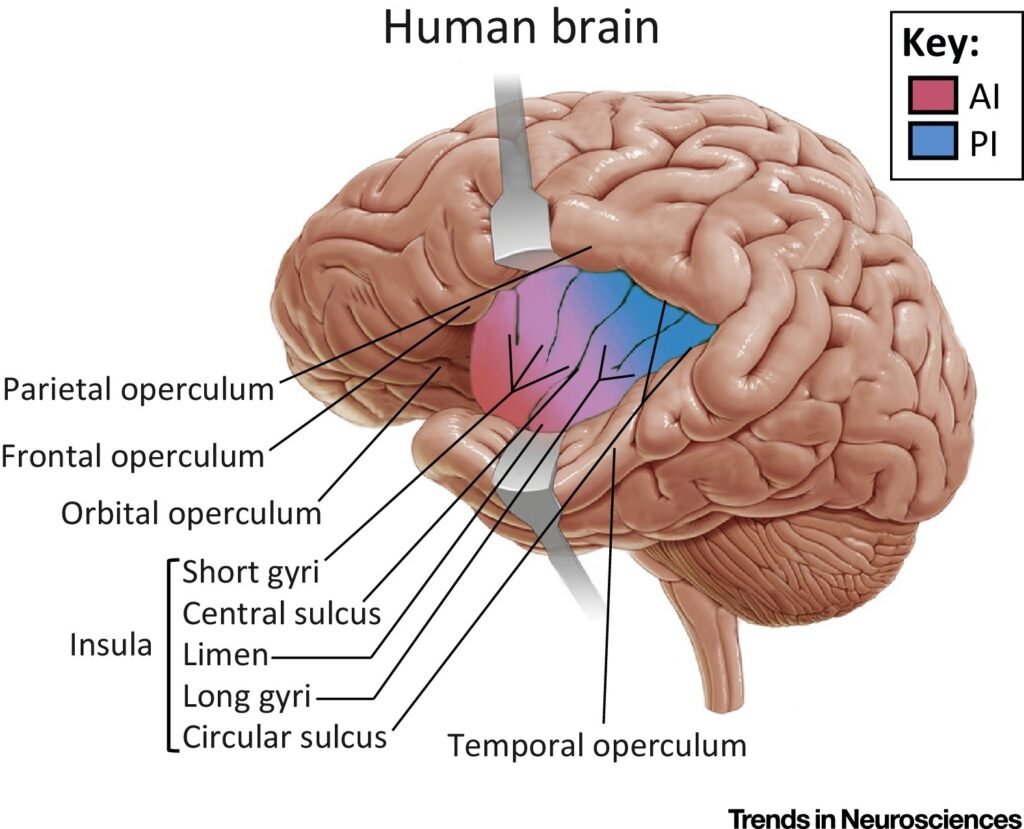
The insula, also known as the insular cortex, is a small but powerful region of the brain deeply embedded in the cerebral cortex. While it might not be as well-known as the prefrontal cortex or hippocampus, the insula is involved in several critical functions, including:
Interoception: The ability to perceive and interpret internal bodily states like hunger, thirst, and pain.
Emotion processing: Helping the brain assign emotional meaning to experiences.
Risk and reward evaluation: Influencing decision-making, particularly in situations involving uncertainty or potential risks.
Craving and addiction behavior: Prior research has established its role in substance use, most notably in cravings.
The insula essentially acts as a bridge between the mind and body. It helps us interpret physical sensations and emotions, a process that often drives behaviors and habits, including drug use. Thus, its role in addiction has become a focal point for scientists.
The study, explored the relationship between insula thickness and cocaine use behavior. Researchers recruited participants with and without prior cocaine use and conducted brain imaging using high-resolution MRI scans.
The results of the study revealed:
These results open up a critical avenue of understanding: How exactly does a thicker insula contribute to increased cocaine use?
One prominent theory suggests that a thicker insula may amplify the brain’s reward response to substances like cocaine. Individuals with a thicker insula might experience stronger cravings or heightened pleasure from drug use, making it harder for them to resist the temptation to indulge.
The insula doesn’t just process physical sensations—it’s also deeply involved in emotional regulation. When this region is structurally thicker, it could interfere with effective regulation of negative emotions like stress, anxiety, or sadness. In turn, individuals may turn to drugs as a coping mechanism.
Because the insula governs our perception of internal bodily states, an overactive or structurally altered insula may create false perceptions, such as an exaggerated sense of craving or discomfort, even when the body doesn’t necessarily need the substance.
The study’s findings underscore the importance of tailoring addiction treatments to individual neurobiological profiles. If insula thickness influences substance use behaviors, brain imaging could become a valuable tool for addiction specialists, helping to identify individuals at higher risk for severe drug use before it becomes problematic.
What This Could Look Like:
Given the insula’s link to craving, treatment modalities like mindfulness-based interventions may prove particularly effective for individuals with thicker insulae. Mindfulness practices help individuals become more attuned to cravings without acting on them, reducing impulsivity associated with substance use.
Implementing routine screenings for structural brain differences, such as through advanced imaging techniques, may allow clinicians to identify at-risk individuals early. This could pave the way for preventive interventions aimed at reducing the likelihood of cocaine use or dependence.
While much of the focus is likely to remain on medical treatments and therapies, lifestyle changes can also play a significant role in supporting the insula’s proper function. Here are several practical strategies:
Mindfulness and meditation strengthen emotional regulation and improve interoceptive awareness, helping reduce the insula’s excessive response to cravings.
Physical activity is well-documented to improve brain function, particularly in regions like the insula and prefrontal cortex. Exercise enhances emotional regulation and curbs impulsive behaviors.
Diets rich in omega-3 fatty acids, antioxidants, and nutrients that support brain health (such as magnesium and B-vitamins) contribute to balanced insular functioning.
Behavioral therapies like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) target emotional dysregulation and impulsivity, directly addressing factors influenced by insular activity.
This groundbreaking study linking thicker insulae to increased cocaine use serves as a reminder of the complex relationship between brain structure and behavior. By understanding the unique ways our brains are wired, we can pave the way for personalized treatment approaches that meet individuals where they are and address their specific challenges.
Here’s what we’ve learned:
As a psychiatric mental health nurse practitioner, I’m thrilled to see how neuroscience continues to unlock new solutions for addiction management. Understanding the biological underpinnings of substance use disorders is essential for creating interventions that are both effective and compassionate.
While we’ve made significant strides in understanding addiction as a brain disorder rather than a moral failing, research like this reminds us that there’s still much to learn. The discovery of the insula’s potential role in cocaine use is a stepping stone toward more comprehensive approaches to addiction care. By leveraging science to inform treatment, we can continue helping individuals break free from the grip of substance use and move toward fulfilling, drug-free lives.
If you or someone you know is struggling with addiction, know that help is available, and treatment options are continually advancing. Reach out to a trusted health professional to explore available resources and begin the path to recovery.
For mental health content that aims to educate, empower, and inspire, stay tuned to this blog!